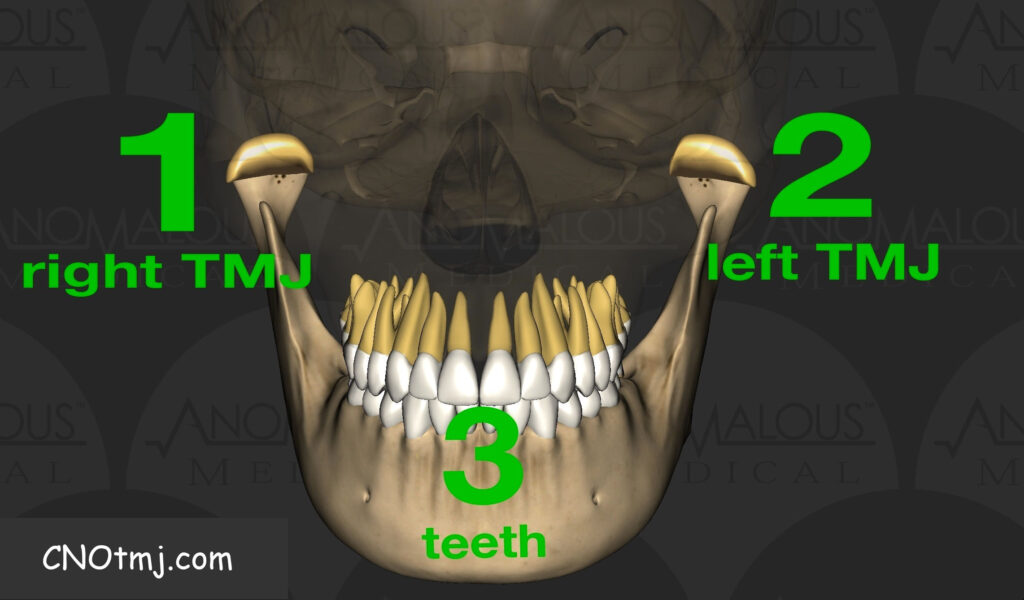
Abstract: MRI imaging is a very useful tool to elucidate the condition of both the hard and soft tissue aspects of the bilateral TMJs. Since the TMJs are essentially 2/3 of the occlusion, essential data may be gleaned from this modern modality to predict occlusal efficacy in the practice of dentistry.
Tipping hydrogen protons with magnetic resonance imaging to visualize internal structures in the practice of dentistry? It seems so niche, but trust me, it is an essential service that all practitioners should at least become introduced to, especially GPs, cosmetic dentists, TMJ specialists, orthodontists, and oral surgeons. Why? It’s simple… You can see more, diagnose more effectively, and help ensure occlusal efficacy of potential treatment(s) in many different areas of dental practice.
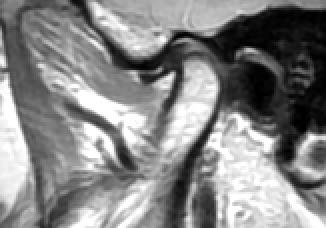
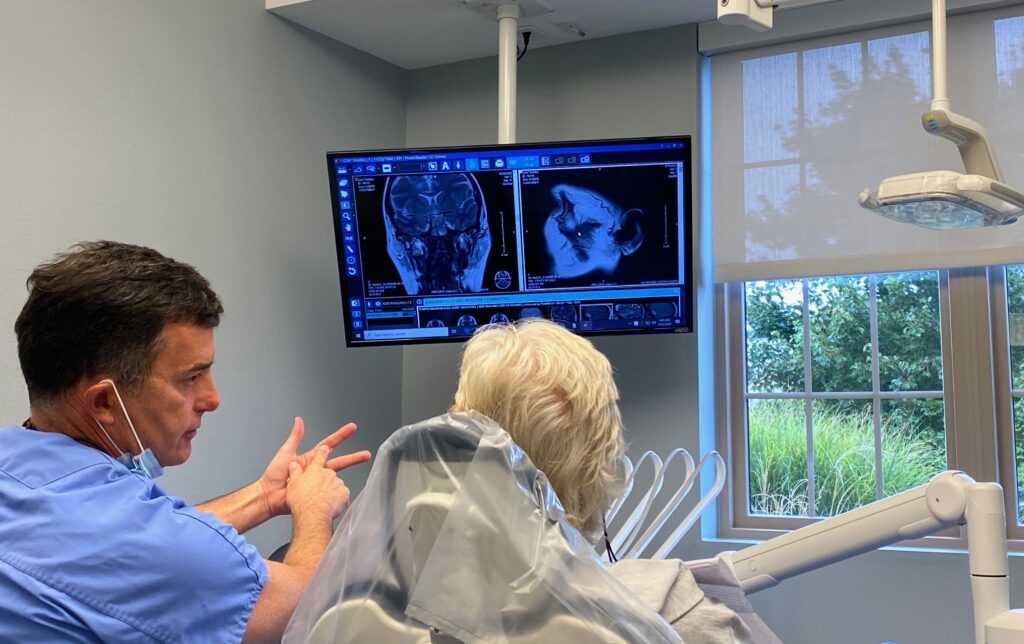
3D MRI imaging is especially useful for visualizing the TMJs in particular, especially when combined with TMJ 3D CBCT imaging. This is extremely relevant to dental practice due to the fact that 2/3 of the occlusion is resultant of both the hard and soft tissue aspects and bilateral condition of the orthopedic TMJs. Understanding the condition, position, and degree of herniation of the TMJ soft-tissue disc as well as the surrounding bony/hard tissue structures allows one to decide if the orthopedic TMJs are relatively stable and adapted, or not. Due to the variant thicknesses of each TMJ soft tissue disc (posterior band thickest, intermediate zone thinnest, anterior band intermediate thickness), displacement of said disc will result in a biomechanical shift in this “hinge” that is the TMJ. This translates into a change in how both the mandible and mandibular dentition interacts with the maxillary dentition. Hence, if a patient does not possess stable joints bilaterally, one cannot expect to possess a stable occlusion if the hard or soft tissue structures of one or both joints are orthopedically unstable. Pearl: the MRI, in particular, allows one to decide if the joints are stable or unstable and maladapted. If either joint is unstable and maladapted, one can expect the occlusion to remain unstable until objective confirmation (via TMJ MRI and CBCT imaging of course) of natural adaptation or surgical intervention occurs.
Common 2D Panoramic imaging is fraught with error due to inherent distortion and lack of measurement capabilities. CBCT allows for an undistorted visualization and potential measurement of hard tissue structures. CBCT standalone allows one to visualize spacing, bony structures, density, and potentially, breaks in the cortical bone. It also lets one calculate lengths and sizes of bony structures, an extremely relevant endeavor to definitively elucidate growth and development issues, or lack thereof. Condylar head surface areas, ramus heights, condylar head to coronoid process relationships; data gleaned from quantifying the aforementioned anatomy is salient to predicting stable orthodontic treatment outcomes, restorative treatment outcomes, and occlusal harmony in general.
CBCT basically shows a knowledgeable practitioner the past and present condition of the TMJs, whilst TMJ MRI imaging shows the practitioner the present and the future, a crystal ball of sorts. Combining the two technologies paves the path for efficacy regarding occlusal outcomes. The MRI can definitively show inflammatory change, both in the hard and soft tissues. An effusion is a pathologic inflammatory change that shows up in the soft tissues, whilst an edema is a pathologic inflammatory change within the hard tissue/bone. MRI can also show the presence or absence of fat within the condylar head, showing the practitioner if the bone is necrotic, or not. Lack of fat within the condylar head is a sign of necrosis, for example, especially if cross-correlation with the MRI does not display sclerosis. If that condylar head does show sclerosis, it likely is not necrotic. If edema happens to be present in either TMJ, for example, the case would be considered unstable since the joint could potentially break down biomechanically, resulting in an unstable occlusion. In a practical sense, restorative or orthodontic movements would not be expected to remain stable in a patient with this sort of orthopedic handicap, made evident thanks to the MRI.
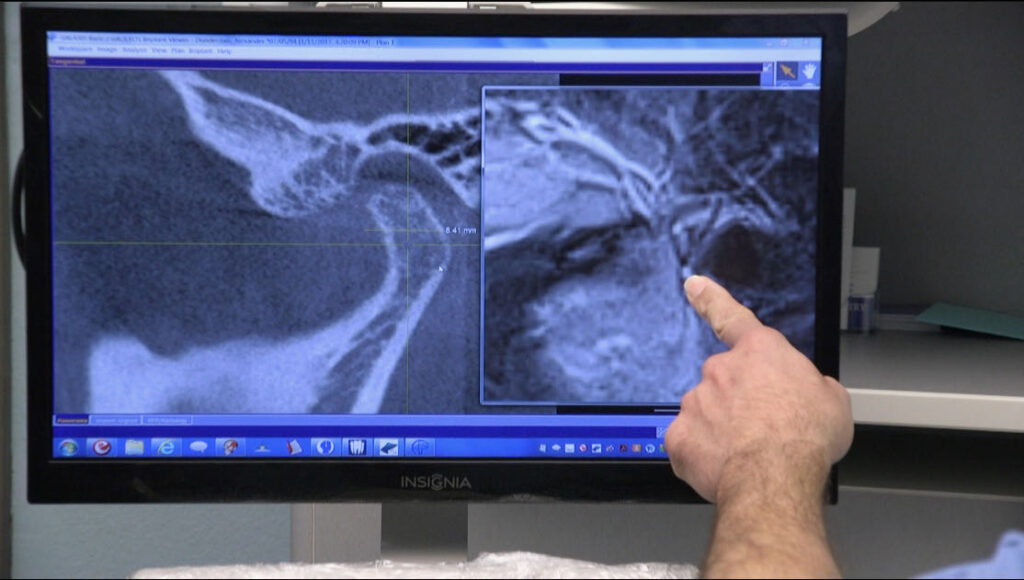
The Center For Neural Occlusion teaches doctors how to order, read, and interpret TMJ MRIs & CBCTs in CNO Level 3, leading practitioners down a path of enlightenment regarding occlusal efficacy. This skillset should be familiar to most all of us practicing dentistry, because after all, we are all dealing with bites.
Measured Matters,