WHAT IS Neural Occlusion Screening (NOS)?
MEASURE THE TMJs MEASURE THE BITE
What We Measure
- Force & Time (T-Scan)
- EMG
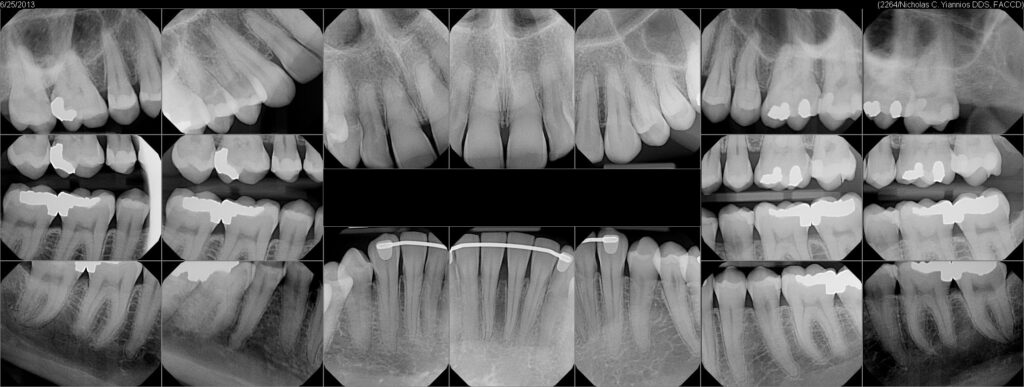
- X-Rays
- Ice Water Swish
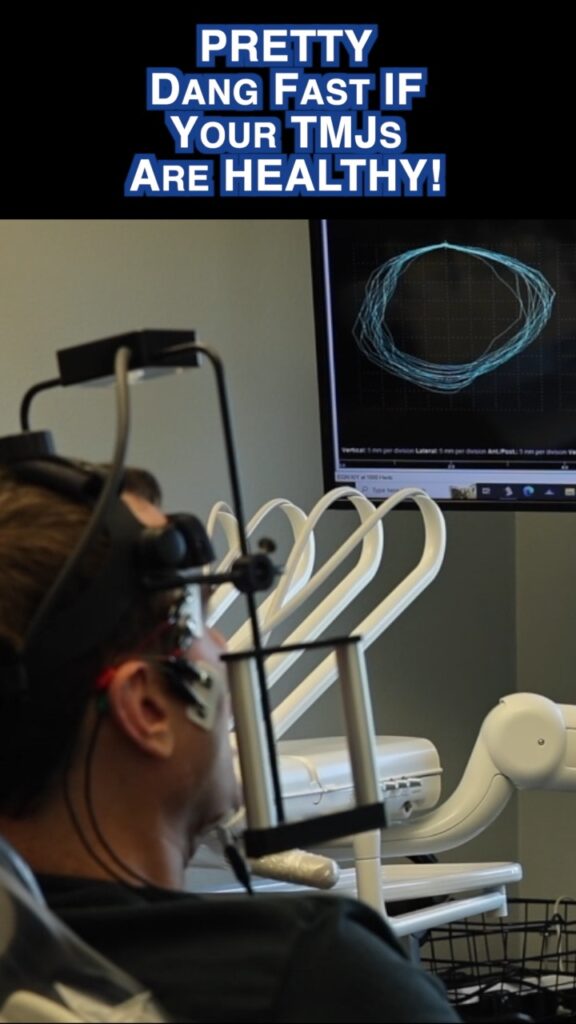
- Jaw Tracking
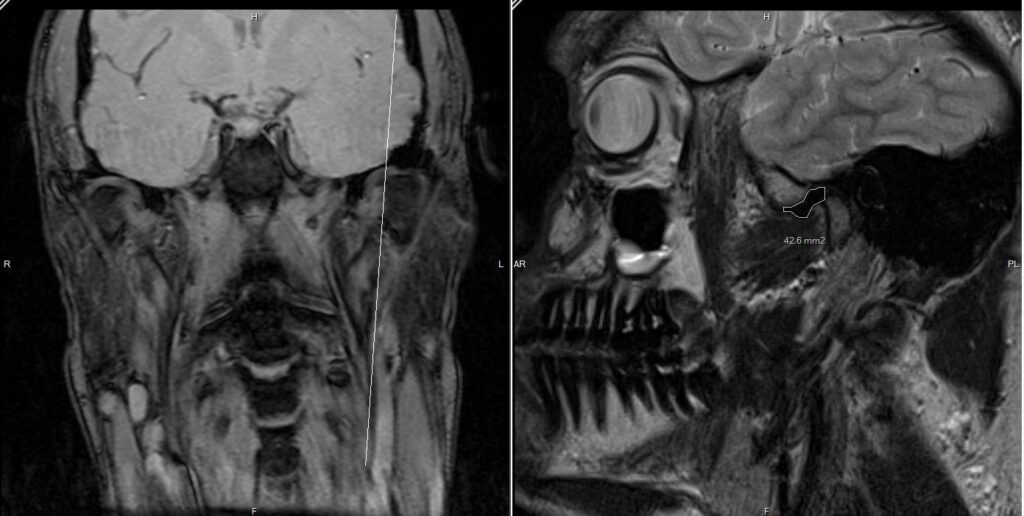
- MRI
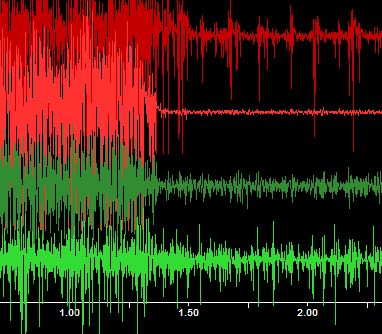
- JVA
- CBCT Scan
- Mastication Analysis
- Sympathetic Blocks
pam tscan
 This device called a T-Scan reads the force and timing of the bite. Placing this into the patient’s mouth it is possible to objectively record and measure the occlusion relative to force and time.
This device called a T-Scan reads the force and timing of the bite. Placing this into the patient’s mouth it is possible to objectively record and measure the occlusion relative to force and time.

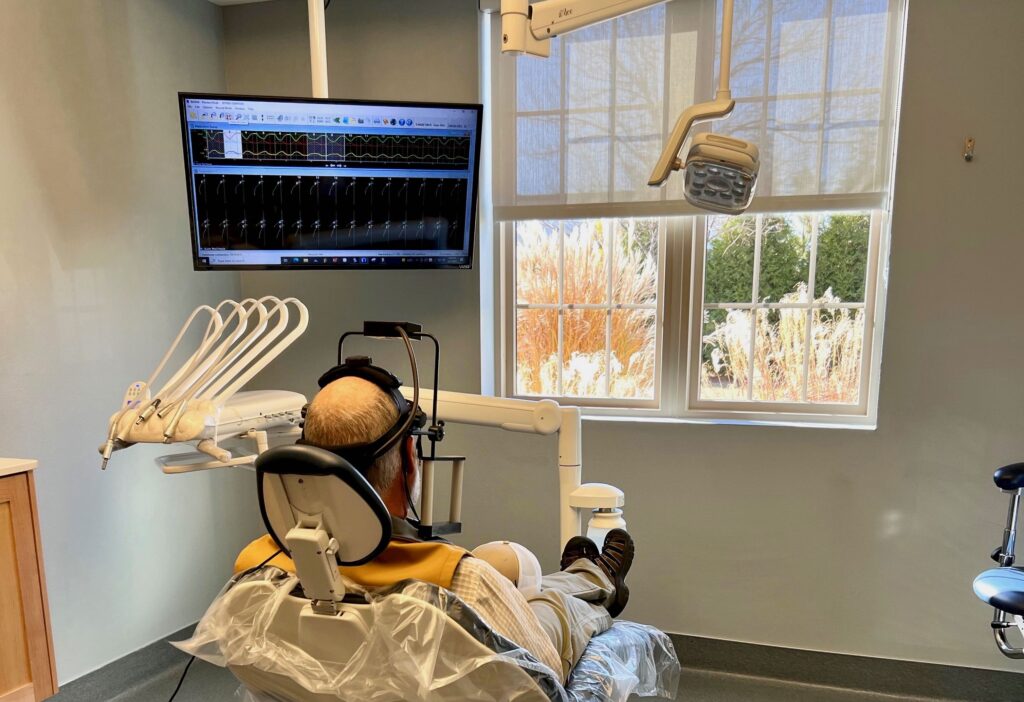
 Electromyography (EMG) is an electrodiagnostic medicine technique for evaluating and recording the electrical activity produced by skeletal muscles in microvoltages. CNO uses the EMG.
Electromyography (EMG) is an electrodiagnostic medicine technique for evaluating and recording the electrical activity produced by skeletal muscles in microvoltages. CNO uses the EMG.
A normal dental checkup is neccesary to rule out basic dental maladies that others may have missed. Sometimes your past dental work is responsible for your TMD issues, or is at least a contributing layer.
Frictional Dental Hypersensitivity (FDH) can occur when the patients muscles are overworking due to a misaligned bite. The patient with a TMD issue solely due to overactive muscles from a bite issue will typically have hypersensitive teeth that shows up when they are challenged with the ice water swish. Once the bite alignment is corrected, the sensitivity will typically go away, permanently. There are neurological reasons for this that are not fully understood, which may relate to the overactivity of the sympathetic branch of the autonomic nervous system. Dr. Nick Yiannios is at the forefront of this particular area of research.

Digital Jaw Tracking technology allows one to objectively and reproducibly track movements of the mandible within the full range of motion. A record is generated, which can be compared to subsequent readings following treatment initiation. Healthy or relatively stable and adapted temporomandibular joints have robust and concentric movements. Unhealthy joints have erratic and non-concentric movements.
Magnetic Resonance Imaging uses magnetic pulses rather than ionizing radiation to study cartilage, fluid, and fat content within both TMJs. An extremely useful tool, MRI often identifies problems that would go completely unnoticed otherwise.
 Joint Vibration Analysis is a screening tool of the TMJ cartilage. JVA is based on simple principles of motion and friction: When smooth surfaces rub together, little friction is created…and little vibration. If these surfaces become rough, as would be the case when the TMJ cartilage is damaged relative to the bone in one or both joints, then the friction and vibration that is created when these surfaces articulate would show up as an aberration in the JVA readings.
Joint Vibration Analysis is a screening tool of the TMJ cartilage. JVA is based on simple principles of motion and friction: When smooth surfaces rub together, little friction is created…and little vibration. If these surfaces become rough, as would be the case when the TMJ cartilage is damaged relative to the bone in one or both joints, then the friction and vibration that is created when these surfaces articulate would show up as an aberration in the JVA readings.
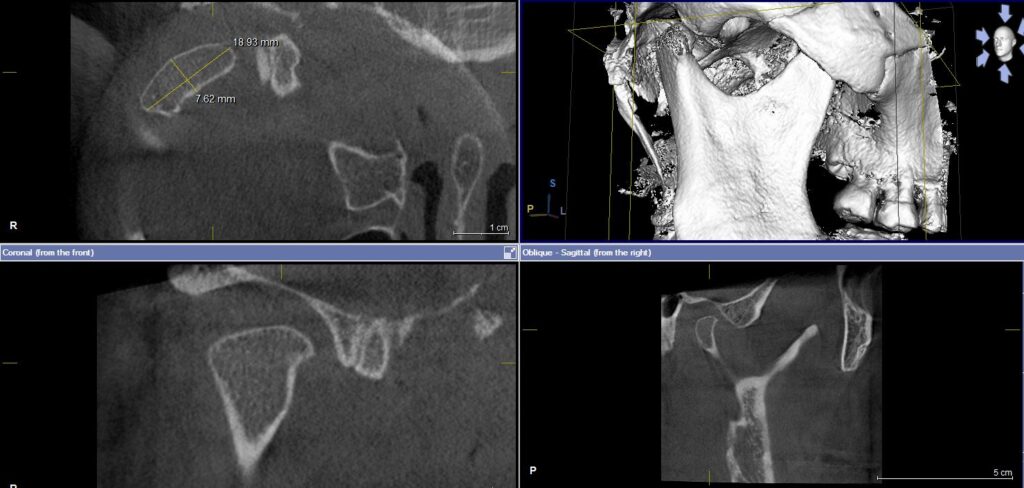
CBCT scan, also called X-ray cone beam computed tomography, is a low-radiation way of studying the bony jaw bone and the skull, objectively elucidating spacing between these bones as well as growth and development issues. It is also very effective at identifying degenerative and arthritic changes that might be taking place within the TMJs as well.
Digital Mastication Analysis involves combining Jaw Tracking with objective electromyography (EMG) technology to repeatedly quantify and record chewing cycles, collecting data that can be compared over passing time after differing treatment plans are iniitiated.
Sympathetic nerves are often responsible for some of the chronic TMJ/D and/or occlusion problems that patients experience. Diagnostic neck blocks using local anesthetic to temporarily block sympathetic nerve flow to lateral face such as via the great auricular nerve as pictured are integral to understanding the source of the problem(s).

CATEGORIZE
CNO Patient Types
Stable Adapted Joints
Objectively Confirmed Healthy TMJs Via 3D TMJ MRI & CBCT Diagnostic Imaging
No Organic Issues
Other MD’s, Neurologists, and Chiropractors Have Ruled Out Other Systemic Issues
The bite is off
Dental Work, Tipped Teeth or Braces Caused This TMD Problem
- This case is very likely to respond to computer-directed bite alignment therapy
- Very Treatable
- High Percentage of Success
Relatively Stable & Adapted Joints
Alignment of the Bite Might Help
Damaged Cartilage
People Are Unaware How Commonly TMJs Are Deranged, But It Is Common
Minor Bone & Cartilage Wear
Usually Due to Damaged Cartilage in the TMJ
- There Is Hope
- Usually At Least Partially Treatable with Computer-Directed Bite Alignment Therapy
- Good Chance Of Partial Success
Unstable Maladapted Joints
Dead Bone
Acute Inflammation & Effusion
- Help is at Hand
- Bite Alignment Treatment Or Manipulation of Any Kind Should Not Be Attempted
- May Need to be Referred for Workup by a TMJ Surgeon
ALIGNMENT
Digitally Directed “Alignment”
IF Indicated
Measured Anterior Guidance Development (MAGD) therapy is a bite/occlusal adjustment procedure used in patients that possess stable and adapted temporomandibular joints (TMJs). Objective confirmation of stable & adapted TMJs leads to predictable outcomes regarding all forms of dental treatment!
When back teeth contact/touch too long in TIME during function, research has shown repeatedly for decades that this neurologically overstimulates muscular contraction within the chewing complex. Many of these muscles, when overworked, become very fatigued and painful, potentially resulting in unexplained headaches and tension within the head and neck. In a practical sense, muscles that overwork chronically can lead to not only broken teeth, but failing dental work as well!
A precise and objective, digitally directed “alignment” of the way the teeth relate to one another over TIME, can reduce this overstimulation of the muscles (in patients with objectively confirmed TMJs), leading to not only a reduction in painful symptoms, but in the likelihood that dental work will not fail over time as well. Prior to bite alteration, it is critical to firstly objectively diagnose the condition of the orthopedic TMJs via gold standard TMJ MRI & CBCT imaging and other metrics that can measure the muscles, the kinesiology and range of motion of the mandible (via Neural Occlusion Screening, or NOS).
Based upon three decades of evidence-based research by Dr. Robert Kerstein and others, computer-directed occlusal adjustments have repeatably been shown to improve many cases of TMD pain of occlusal genesis, specifically in cases which possess relatively orthopedically stable and adapted TMJs. In such cases, removing pathological excursive occlusal contacts based upon precise and digitally-identified contacts in the dynamic occlusion will often palliate chronic muscular TMD pain, and will often simultaneously allow the dental practitioner to improve the integrity of not only the dentition, but properly placed restorative treatments and orthodontic movements as well. Those doctors that have trained up to CNO level 3 (MCNO) are particularly adept at diagnosing and treating appropriate cases such as these.
CLICK THE ABOVE SECTION FOR SAMPLE VIDEO OF NOS & MAGD TREATMENT OF A TMJ/D PATIENT



